Echoes of the Past, Realities of Today
The mere mention of “bubonic plague” conjures chilling images of medieval pandemics, mass graves, and an era shrouded in fear. Known historically as the “Black Death,” this formidable disease once decimated populations across continents, fundamentally reshaping human history. Yet, centuries later, whispers of the plague continue to surface, not just in history books, but in headlines from various parts of the world, including recent reports from the United States. This raises a crucial question: Is the Black Death still a threat? The unequivocal answer is yes, albeit a different kind of threat than its historical counterpart.
While modern medicine has largely tamed its devastating impact, bubonic plague remains an active, though rare, bacterial infection with the potential for serious consequences if left untreated. Understanding its origins, how it spreads, its symptoms, and crucially, how to prevent it, is paramount in an interconnected world. This comprehensive guide aims to peel back the layers of myth and misinformation surrounding the bubonic plague, offering an SEO-rich, human-centric perspective on its historical significance, current epidemiology, and essential safety measures. Join us as we navigate the complexities of this ancient foe in a contemporary context, ensuring you’re equipped with the knowledge to stay safe and informed.

What is Bubonic Plague? Unpacking the Disease
To truly grasp the bubonic plague, we must first understand its fundamental nature. It is one of three main forms of plague, all caused by the bacterium Yersinia pestis. This formidable pathogen primarily circulates among small mammals and their fleas, particularly rodents.
The Culprit: Yersinia pestis
Yersinia pestis is a Gram-negative, rod-shaped bacterium belonging to the family Enterobacteriaceae. It’s a highly virulent pathogen, capable of causing rapid and severe illness in humans. Its ability to thrive in both rodent hosts and flea vectors makes it particularly effective at transmission.
Types of Plague: Beyond Bubonic
While bubonic plague is the most common form, it’s essential to distinguish it from its equally dangerous siblings:
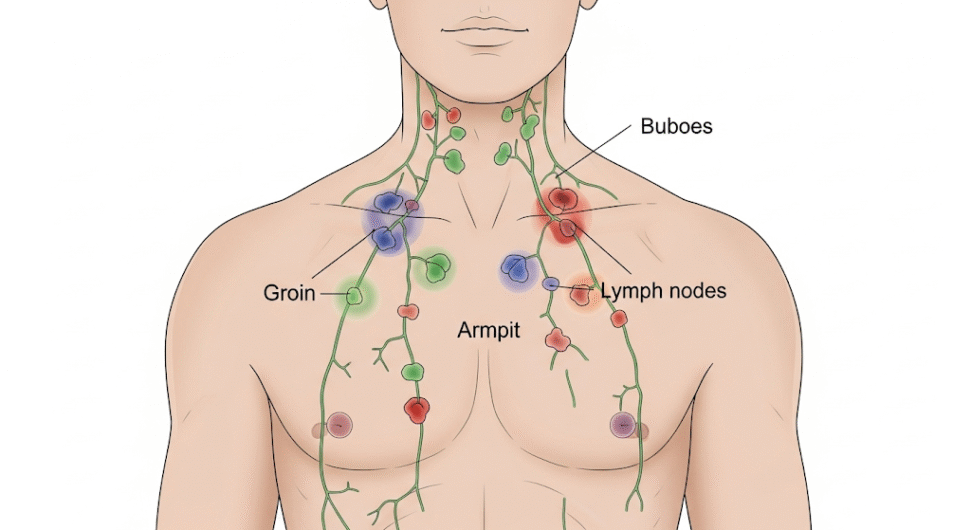
- Bubonic Plague: This is the most prevalent form, accounting for over 80% of U.S. cases. It typically results from the bite of an infected flea. The bacteria multiply in the lymph nodes closest to where the bacteria entered the body, causing them to swell painfully. These swollen lymph nodes are known as “buboes,” giving the disease its name.
- Septicemic Plague: This occurs when the Yersinia pestis bacteria multiply in the bloodstream, either as a progression of bubonic plague or, less commonly, as a primary infection. It can cause fever, chills, extreme weakness, abdominal pain, shock, and bleeding into the skin and other organs.
- Pneumonic Plague: The most severe and, importantly, the only form of plague that can spread directly from person to person through airborne droplets. This form affects the lungs and can be primary (inhaled) or secondary (developing from untreated bubonic or septicemic plague). Symptoms include fever, headache, weakness, and rapidly developing pneumonia with shortness of breath, chest pain, cough, and bloody or watery sputum. This is the form that often causes public health alerts due to its contagious nature.
How it Spreads: From Fleas to Humans
The primary mode of transmission for bubonic plague to humans is through the bite of an infected flea that has previously fed on an infected rodent. However, direct contact with infected animals (including pets like cats and dogs that may carry infected fleas or have eaten infected rodents), inhaling infectious droplets from a person or animal with pneumonic plague, or handling infected animal tissues can also lead to infection. The bacterium cannot be transmitted from person to person for bubonic or septicemic plague.
A Glimpse into History: The Black Death and Its Legacy
The history of the bubonic plague is not just a medical narrative; it’s a global epic that has shaped societies, economies, and even cultures. The most infamous episode, the Black Death of the 14th century, remains a stark reminder of disease’s power.
The Black Death: A Global Cataclysm
Originating likely in Central Asia, the Black Death swept across Asia, Europe, and Africa in the mid-14th century, leaving an unimaginable trail of death. Estimates suggest it killed 30-50% of Europe’s population, profoundly impacting medieval society. Its rapid spread was facilitated by trade routes and the dense urban populations of the time, coupled with poor sanitation.
Subsequent Epidemics and Declines
While the Black Death was the most devastating, subsequent waves of plague continued to strike various regions for centuries, though typically less severely. Over time, factors such as improved public health, sanitation, and eventually, the discovery of antibiotics, led to a significant decline in large-scale plague epidemics in many parts of the world.
Lessons Learned: Public Health’s Evolution
The historical struggle against plague catalyzed significant advancements in public health practices, including quarantine measures, improved waste management, and a greater understanding of disease transmission. The legacy of the Black Death continues to inform our approaches to infectious disease control today.
Bubonic Plague Today: A Modern Perspective
Despite its historical notoriety, bubonic plague is not a relic of the past. It continues to exist as an endemic disease in certain parts of the world, including rural areas of the Western United States.
Global Hotspots: Where Plague Persists
Since the 1990s, the majority of human plague cases worldwide have occurred in Africa, particularly in the Democratic Republic of Congo, Madagascar, and Peru. Smaller outbreaks and sporadic cases also occur in Asia and South America. These cases primarily affect people living in small towns, villages, or agricultural areas, where contact with infected wild rodents and their fleas is more common.
The U.S. Context: A Persistent Rural Threat
In the United States, an average of about seven human plague cases are reported each year. The vast majority of these cases, over 80%, are bubonic plague. These cases are concentrated primarily in the western U.S., particularly in:
- Northern New Mexico
- Arizona
- Southern Colorado
- California
- Southern Oregon
- Far western Nevada
The last urban plague epidemic in the U.S. occurred in Los Angeles from 1924-1925. Following this, the disease became entrenched in rural rodent populations. Cases in the eastern U.S. are extremely rare and are typically linked to travel from the western U states or laboratory exposure.
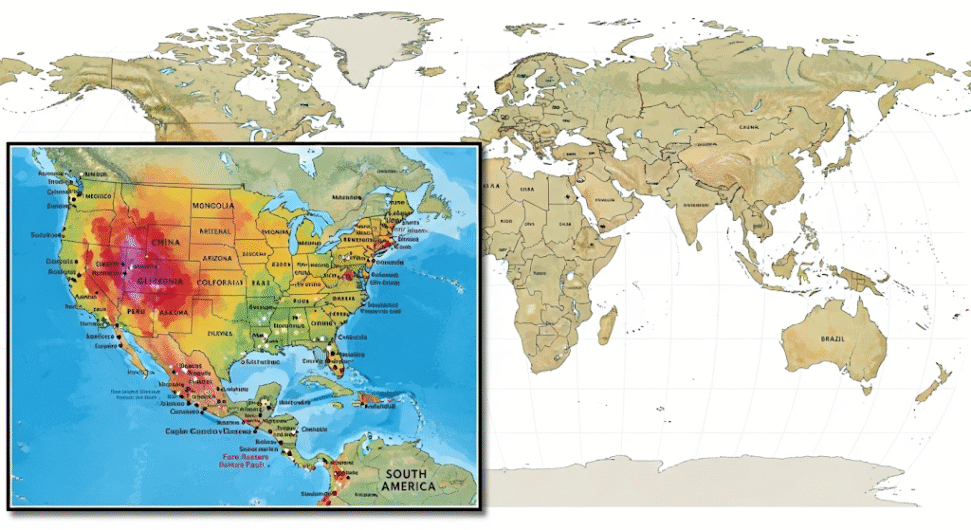
For detailed maps and statistics on plague cases worldwide and in the U.S., visit the CDC’s Plague Maps & Statistics page.
Recognizing the Signs: Symptoms of Bubonic Plague
Early detection and treatment are critical for surviving bubonic plague. Knowing the symptoms is the first step in seeking timely medical attention.
Typical Symptoms of Bubonic Plague
Symptoms usually appear suddenly, typically within 2 to 6 days after exposure to the bacteria. Key signs include:
- Fever: Often high (102°F/39°C or higher).
- Chills: Shivering often accompanies the fever.
- Extreme Weakness and Malaise: A general feeling of being unwell and severely fatigued.
- Headache: Often severe.
- Muscle Aches: Body aches are common.
- Buboes: The hallmark symptom of bubonic plague. These are swollen, painful, and tender lymph nodes, typically found in the groin, armpit, or neck area. They can range in size from a chicken egg to an apple. The skin over the bubo may appear reddish and stretched.
Progression to Other Forms (If Untreated)
If bubonic plague is not treated promptly with antibiotics, the bacteria can spread from the lymph nodes into the bloodstream, leading to septicemic plague, or to the lungs, resulting in pneumonic plague. The development of septicemic or pneumonic plague significantly increases the severity of the illness and the risk of death.
When to Seek Medical Attention
Given the rapid progression of the disease, anyone experiencing these symptoms, especially if they have recently traveled to endemic areas, been exposed to rodents or fleas, or have been in contact with someone diagnosed with plague, should seek immediate medical attention. Early diagnosis and treatment are crucial for a positive outcome.
Prevention is Key: Staying Safe from Bubonic Plague
While rare, bubonic plague is preventable. Implementing simple precautions, especially if you live in or visit endemic areas, can significantly reduce your risk of exposure.
Avoiding Flea Bites: Your First Line of Defense
Since infected fleas are the primary vector, preventing flea bites is paramount:
- Use Insect Repellent: When outdoors, especially in areas where plague is known to occur, use insect repellents containing DEET or other EPA-approved active ingredients on skin and clothing.
- Protective Clothing: Wear long pants and long-sleeved shirts when in areas where rodent fleas may be present. Tuck pants into socks to prevent fleas from gaining access to skin.
- Treat Pets for Fleas: Regularly treat dogs and cats for fleas, especially if they spend time outdoors. Consult your veterinarian for appropriate flea control products. Do not allow sick pets to sleep in your bed.
- Avoid Rodent Habitats: Stay away from sick or dead animals, particularly rodents (squirrels, chipmunks, prairie dogs, rats, mice). Do not handle them with bare hands.
Managing Rodent Populations Around Your Home
Reducing rodent populations near your living spaces is crucial:
- Eliminate Food Sources: Store food in rodent-proof containers. Dispose of garbage in sealed bins.
- Seal Entry Points: Seal holes and cracks in foundations, walls, and around pipes to prevent rodents from entering your home.
- Clear Debris: Remove brush, rock piles, junk, and potential rodent nesting sites from around your home and yard.
Handling Animals and Pet Precautions
- Wear Gloves: If you must handle sick or dead animals, wear gloves.
- Keep Pets Leashed: When hiking or camping, keep pets on a leash to prevent them from exploring rodent burrows or interacting with wild animals.
- Veterinary Care: If your pet becomes ill with a sudden fever and lethargy, especially if they live in an endemic area, seek veterinary care immediately and inform your vet about potential plague exposure.
Travel Precautions
- Research Endemic Areas: Before traveling to known plague-endemic regions, familiarize yourself with local risks and take appropriate precautions.
- Be Aware of Symptoms: If you develop symptoms after returning from an endemic area, seek medical attention and inform your doctor about your travel history.

Diagnosis and Treatment: Modern Medicine’s Response
Thanks to advancements in medical science, bubonic plague, while serious, is treatable, especially when diagnosed early.
Diagnosing Plague: A Race Against Time
Diagnosis relies on identifying the Yersinia pestis bacterium from patient samples. This typically involves:
- Clinical Suspicion: Based on symptoms and exposure history.
- Laboratory Tests:
- Bubo Aspirate: Fluid from a bubo (lymph node) is aspirated and examined under a microscope for the characteristic bacteria.
- Blood Samples: Blood cultures can identify the bacteria, particularly in septicemic plague.
- Sputum Samples: For suspected pneumonic plague, sputum (phlegm) is collected and analyzed.
- Rapid Diagnostic Tests: Available in some settings, these tests can quickly detect plague antigens.
The Power of Antibiotics
Antibiotics are highly effective in treating plague. Treatment should begin as soon as plague is suspected, without waiting for laboratory confirmation, due to the rapid progression of the disease. Common antibiotics used include:
- Gentamicin
- Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin)
- Doxycycline
- Chloramphenicol (often used for pneumonic plague or cases with central nervous system involvement)
Early antibiotic treatment dramatically reduces the mortality rate from bubonic plague. Untreated plague can have a fatality rate of 30-60%.
Supportive Care and Prognosis
Beyond antibiotics, supportive care is essential, including fluid management, pain relief, and fever reduction. With timely and appropriate treatment, most patients with bubonic plague make a full recovery. However, complications can arise, especially if treatment is delay

Learn more about the specific diagnostic methods and treatment protocols for plague from the World Health Organization (WHO) website.
Public Health Surveillance and Global Efforts
The rarity of plague in many developed nations doesn’t mean public health authorities are complacent. Robust surveillance systems and international collaboration are vital to monitoring and controlling this disease.
Surveillance Systems: Keeping an Eye on the Threat
Public health agencies, like the Centers for Disease Control and Prevention (CDC) in the U.S. and national health ministries globally, maintain active surveillance programs. These programs involve:
- Monitoring Rodent Populations: Tracking rodent populations and testing them for the Yersinia pestis bacterium.
- Human Case Reporting: Prompt reporting of suspected and confirmed human cases to national and international health organizations.
- Contact Tracing: For pneumonic plague cases, identifying and monitoring contacts to prevent further spread.
- Environmental Monitoring: Assessing environmental factors that might increase the risk of plague outbreaks.
International Collaboration and Preparedness
Organizations like the World Health Organization (WHO) play a critical role in coordinating global efforts to combat plague. This includes:
- Providing Guidelines: Developing and disseminating international guidelines for plague surveillance, diagnosis, and treatment.
- Supporting Endemic Countries: Offering technical assistance and resources to countries where plague is endemic.
- Research and Development: Supporting research into new diagnostic tools, treatments, and vaccines.
- Emergency Response: Coordinating rapid response teams in the event of outbreaks.
The Importance of Public Awareness
Educating the public about plague risks and prevention measures is a cornerstone of effective control. Campaigns often focus on areas where the disease is endemic, advising residents on how to reduce their exposure to rodents and fleas.

For broader information on infectious disease surveillance and global health security, explore resources from the Council on Foreign Relations on Global Health.
Vigilance in the Face of an Ancient Foe
The bubonic plague, an infamous disease of antiquity, continues to remind us that even the most historical threats can persist in the modern world. While no longer the rampant killer it once was, its presence, particularly in certain rural areas, underscores the importance of continuous vigilance, public health awareness, and scientific advancements.
By understanding how Yersinia pestis operates, recognizing the symptoms of infection, and adopting simple, effective prevention strategies, individuals can significantly reduce their risk. Moreover, the tireless efforts of public health professionals and international organizations in surveillance, research, and response are vital in keeping this ancient foe at bay.
The narrative of the bubonic plague is a testament to both the fragility of human life in the face of microscopic threats and the remarkable resilience and ingenuity of scientific and medical endeavors. As we move forward, remaining informed and proactive is our best defense against diseases that echo from the past, ensuring that the Black Death remains largely confined to the pages of history, rather than the headlines of tomorrow.